Overview:
As the COVID-19 pandemic grinds on in our communities, doctors’ understandings of the origin, signs and symptoms, treatment, recovery and aftermath of the viral infection is growing at a tremendous rate. ENTA doctors who are on the front lines of this disease have come face-to-face (literally—though with N95 masks and sometimes face shields on!) with some of the long-term effects of this virus. We pass some current understanding and theories on to you.
Early Signs of Infection:
The earliest sign of COVID-19 infection in many, but not all, individuals is the loss of smell and/or taste. This usually precedes the typical fever, cough, shortness of breath, and sore throat that occur in people who become acutely ill of the disease. Indeed, some people only have loss of smell or alteration of taste as their symptoms and never become acutely ill.
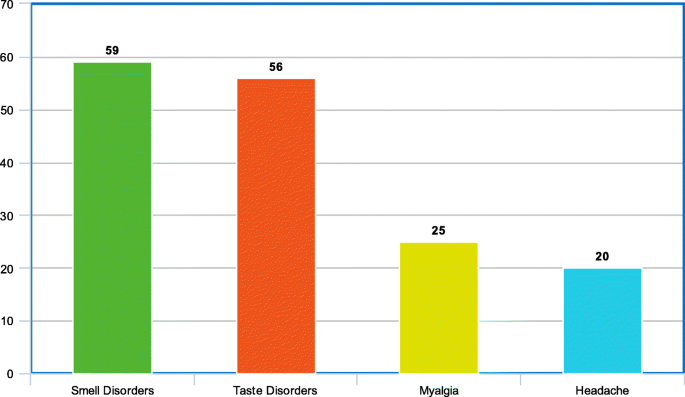
Percentage of COVID-19 patient who exhibit four common symptoms
Invasion of the Virus:
It is well-established that the coronavirus causing COVID-19 incubates for several days in the nasal cavity and nasopharynx (the back part of the nose). This is the reason for the nasal swab test.
Evidence suggests that the virus directly invades the central nervous system through one of two speculative mechanisms: neuronal (nerve) spread and hematogenous (blood) spread. This is believed to be a cause of the COVID-19 symptoms of viral encephalitis, loss of cognitive function, peripheral neuropathies, and destruction of respiratory drive neurons (“Ondine’s Curse”). The destruction of respiratory drive neurons, in conjunction with lung damage, is thought to be one of the reasons it is so difficult to wean some patients off ventilators.
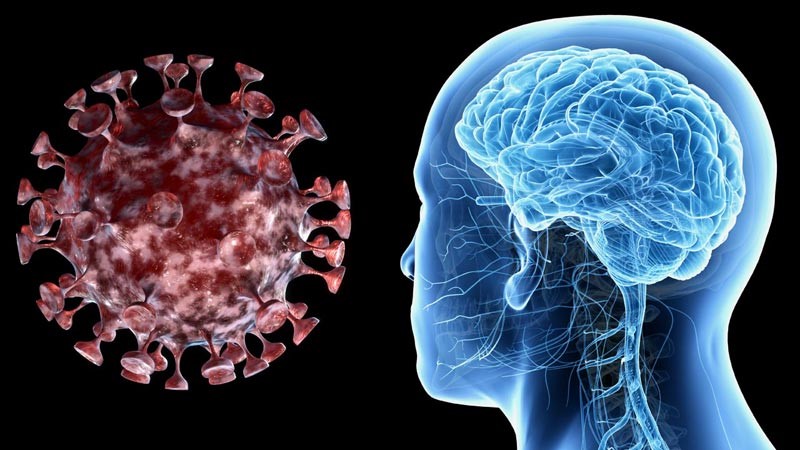
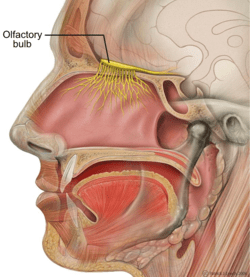
The most exposed portion of our central nervous system is our olfactory bulb, the sense organ for smell. Virus particles have been isolated from the olfactory bulb, olfactory nerve, central nervous system neuronal cells, and cerebrospinal fluid. The post-mortem evidence that only the nerve (neuronal) cells and not the supporting (glial) cells contain virus supports the neuronal theory of spread, such that the virus marches up nerve-by-nerve into the brain. Once in the brain, the virus has the propensity to travel to parts of the brain called the thalamus and the brainstem. Previously, this mechanism of spread has been established for other coronaviruses: SARS(severe acute respiratory syndrome)-CoV-1 and MERS(Middle East respiratory syndrome)-CoV.
From the perspective of brainstem damage, many ENT functions such as smell, taste, balance, vertigo, speech, salivation, and swallowing originate and are mediated in the brainstem—so in theory (not proven)—these functions could be affected. Some of these manifestations are thought to be mediated through the vagus (Latin: “wanderer”) nerve that transmits signals controlling voice production, heart rate, gastric acid production, etc. This dysfunction directly or indirectly affects many symptoms that are commonly seen by ENTs.
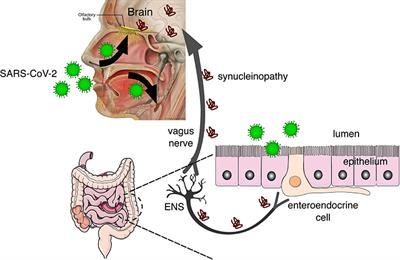
Proposed pathway of COVID-19 spread through central nervous system and the gut.
Vascular and Immunologic Damage:
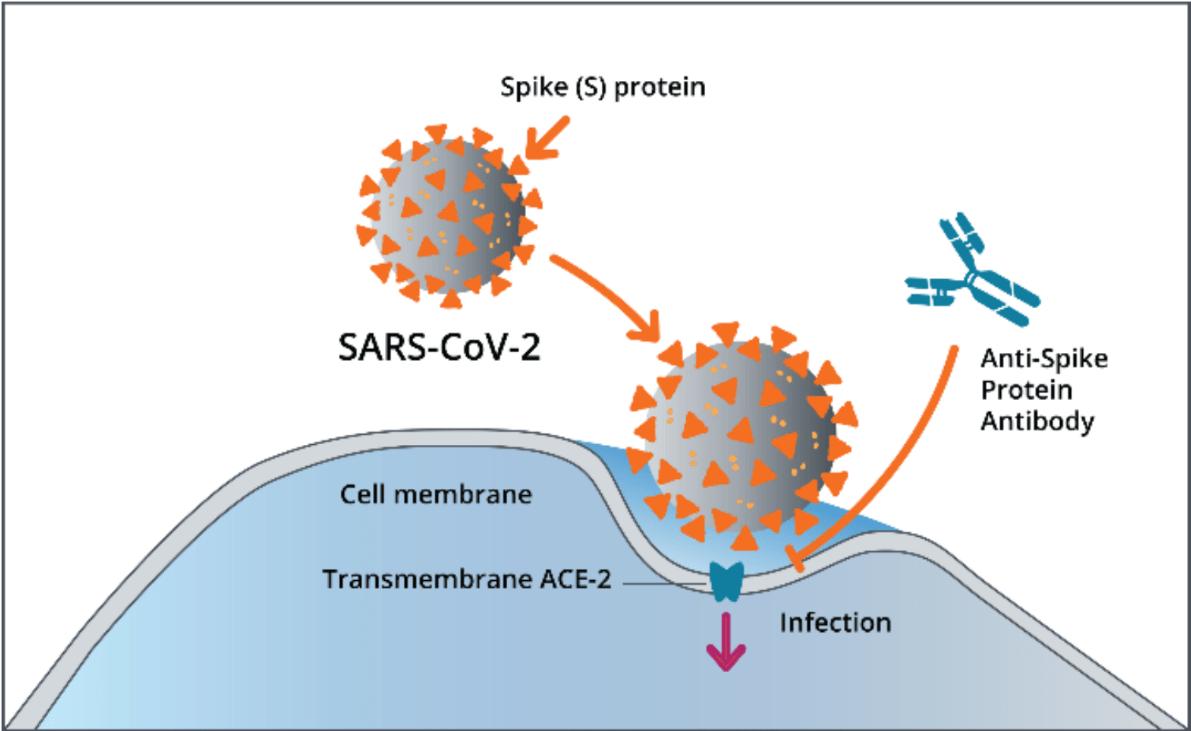
COVID-19 can damage blood vessels walls and cause a damaging immune over-reaction (“cytokine storm”). All coronaviruses contain nucleotide fragments that code for a protein called “spike protein” that allows the virus to attach to and enter a cell via the cell’s ACE2 receptor:
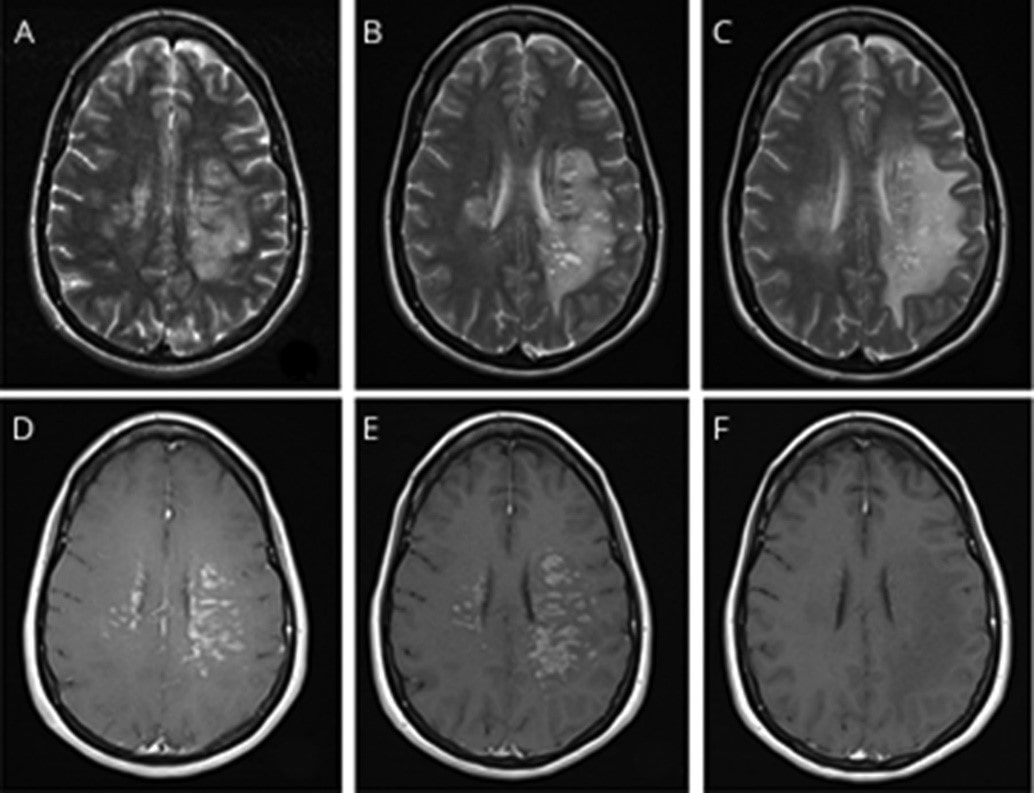
Brain vessel damage due to COVID-19 and resolution after COVID treatment
Consequences of COVID-19
The long-term consequences of COVID-19 fall into 4 main categories: Pulmonary, Cardiac, Neurological, and Psychiatric. Some patients have recognized that they have not returned to their original state of health weeks or months following original infection. They have coined the phrase “Long-haul COVID” defining their continuing medical problems.
Cardiac and pulmonary consequences are beyond the scope of this short blog.
The neurological and neuropsychiatric consequences can occur after or during acute coronavirus infection and are independent of the severity of the initial infection. The following graph displays the age and percentage of COVID patients that experience these symptoms:
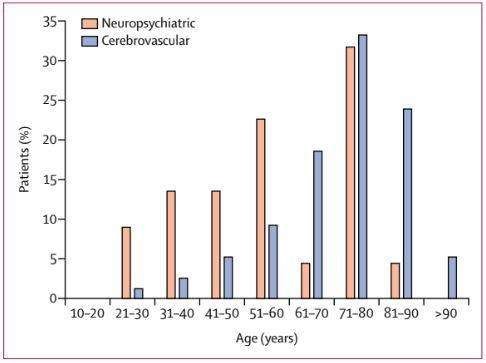
At last estimate, 5% to 35% of COVID patients suffer these symptoms. A June 2020 paper in Neurology reported that some patients with COVID-19 illness exhibit signs of brain damage or brain injury (though authors believe this is uncommon). These symptoms could include coma, seizures, limb sensory abnormalities, paralysis, decreased consciousness and decreased cognition. The neuropsychiatric fallout of COVID-19 has been PTSD, fatigue, cognitive impairments, decreased memory, decreased attention, and psychiatric impairment. It is unknown whether most patients will gradually recover or whether some will have lifetime effects.
Help is on the way!
“Science is telling us that we can do phenomenal things if we put our minds to it.”
--Anthony S. Fauci, MD
In response to these “long-haul COVID” symptoms, many on-line blogs have arisen so that people can describe symptoms, find support, and identify help resources. My patients have largely benefited from this ability to compare experiences with others. Of course, you should discuss your health questions and symptoms with your personal physician as well!
The Mt. Sinai Hospital in New York City in mid-May established a multi-disciplinary group of specialists in order to address these long-haul COVID symptoms. This is the Center for Post-COVID Care. For information about the Mount Sinai Center for Post-COVID Care, visit https://www.mountsinai.org/about/covid19/center-post-covid-care or call (212) 844-6300.
Find an ENT & Allergy Associates Doctor Near You, or Explore More Blog Topics
