September 28th is National Penicillin Allergy Day. On this date in 1928, Alexander Flemming discovered penicillin! According to NationalPenicillinAllergyDay.com, "National Penicillin Allergy Day is an annual celebration to raise awareness around the impact of carrying a penicillin allergy label and how it affects a patient’s healthcare treatment. It focuses on the importance of knowing a patient’s true allergy history while offering tools, activities, and ideas to help create penicillin allergy awareness throughout healthcare offices, facilities, and communities."
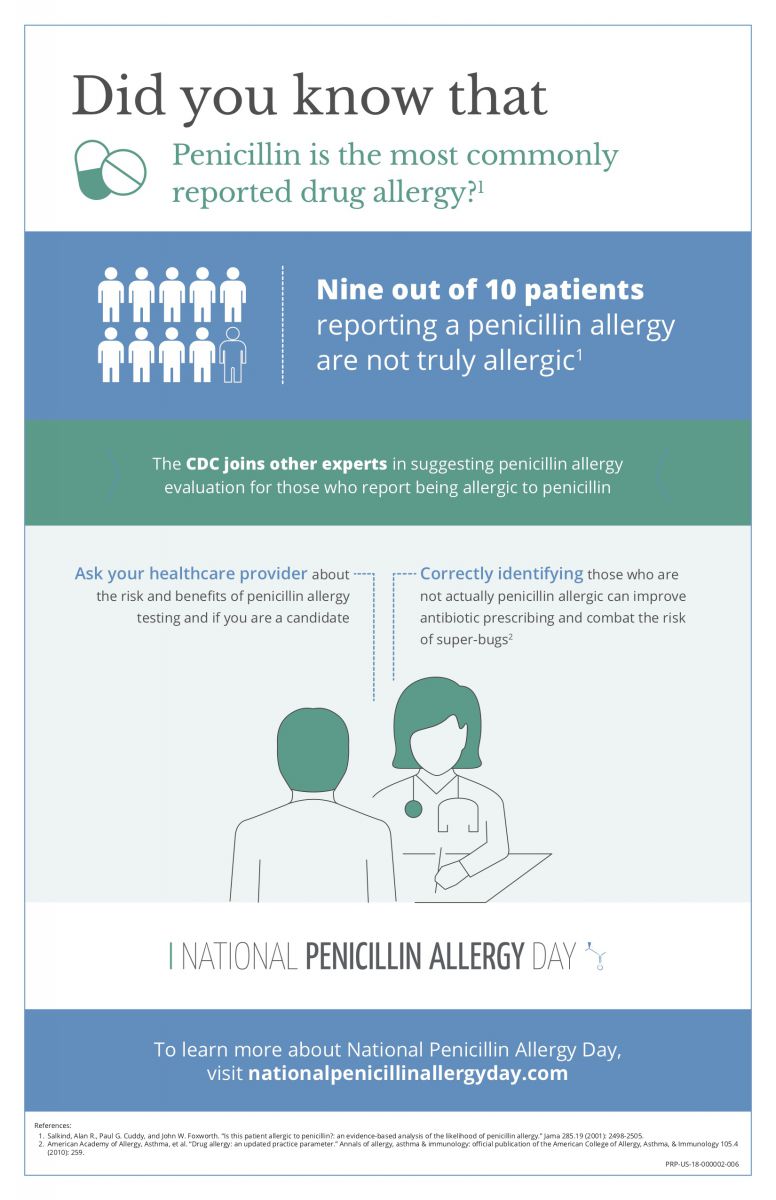
Approximately 10% of the population reports a penicillin allergy. However, over 90% of these individuals will tolerate penicillin after undergoing evaluation. Patients are frequently diagnosed with a penicillin allergy during childhood and a viral infection may be the cause of the rash or hives rather than a drug allergy. For patients with a true drug allergy, 50% will lose the allergy within 5 years.
A penicillin allergy label increases the risk for healthcare-associated infections and potentially poorer infection outcomes as well as increased antibiotic resistance, healthcare utilization, and cost. Less than 1% of the eligible population receives penicillin allergy evaluation.
Katherine Szema, an allergist in our Shrewsbury, NJ office, states that "patients who have a drug reaction history of itching, rash, hives, swelling, shortness of breath, or low blood pressure after exposure to penicillin are candidates for evaluation by an allergist/immunologist who will obtain a careful history and perform allergy procedures, such as skin testing and/or a test dose, if indicated."
Why is correctly identifying those who are not actually allergic to penicillin so important?
- Inaccurate diagnosis of penicillin allergy can adversely impact medical costs for both patients and healthcare systems: research shows that antibiotic costs for patients reporting penicillin allergies are up to 63% higher than for those who do not report being penicillin-allergic.3
- Patients labeled penicillin-allergic may have a threefold increased risk of adverse events (ADE).4 In the hospital setting, history of penicillin allergy translates to about 10% more hospital days,3 30% higher incidence of VRE infections, 23% higher incidence of C difficile infections, and 14% higher incidence of MRSA infections.5
- Correctly identifying those who are not actually allergic can improve antibiotic prescribing and combat the risk of super-bugs by allowing patients access to safer, less toxic antibiotics.4 By some estimates, up to half of all hospitalized patients in the US receive antibiotics and up to half of antimicrobial use may be inappropriate.6 There is a causal relationship between inappropriate antimicrobial use and resistance; changes in antimicrobial use lead to parallel changes in the prevalence of resistance.1
With statistics this compelling, it's important for patients and providers to know the facts about penicillin allergies.
For these reasons, Sept. 28—the date Alexander Fleming discovered penicillin in 1928—has been designated National Penicillin Allergy Day.
Source: https://nationalpenicillinallergyday.com/
Find an ENT & Allergy Associates Doctor Near You, or Explore More Blog Topics
