Specialists in obstructive sleep apnea medicine and surgery at ENT and Allergy Associates, LLP have recognized the long-underappreciated role of sleep and are in the forefront of developing new perspectives, diagnosis modalities, treatment paradigms, and minimally invasive procedures for the benefit of our affected patients.
Sleep, the other third of our life.
Sleep has traditionally been regarded as the “blank” 1/3 of our time on this earth. In the past two decades, this idea has been turned on its head, and an entire field of study has evolved to understand the important contribution that quality sleep makes to our well-being.
The American Academy of Sleep Medicine indicates 30 million adults have obstructive sleep apnea, 411 billion dollars of economic loss are due to insufficient sleep, 30% of adults complain of insomnia, and 328,000 motor vehicle accidents per year are caused by drowsy driving.
Disordered and apneic sleep places a tremendous burden on our hearts, blood vessels, lungs, and brain, and contributes to hypertension, heart attack, heart failure, obesity, diabetes, gastric reflux (GERD), pulmonary hypertension, stroke, erectile dysfunction, memory loss, accidents, depression, anxiety, inattention, poor work performance, and dementia.
Snoring isn’t funny
While not everyone who snores has sleep apnea, virtually everyone with sleep apnea snores. At ENTA we use a simple mnemonic to identify those individuals with a moderate or high risk of OSA, who are then offered additional evaluation. The mnemonic is: STOP-BANG:
Those with a STOP-BANG score of 0-3 are at low risk for OSA. If the STOP-BANG score is 4-8, then the individual is at high risk for OSA. For those individuals, a Home Sleep Study (HST) is recommended. An HST measures the physiologic parameters that are most critical in the evaluation of OSA. This study is done in the comfort and privacy of your own bed, and the device is mailed or delivered to the sleep lab in the morning. From that data, a further lab study or—more likely--a treatment plan is devised.
- Snoring
- Tired or fatigued during the day
- Observed to halt breathing at night.
- Pressure: High blood pressure
- BMI > 35
- Age > 50
- Neck size > 17 inches.
- Gender - Male
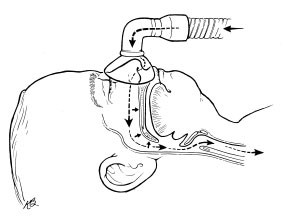
Long considered the “gold standard” of treatment, nasal Continuous Positive Airway Pressure (CPAP), is traditionally the first stage of treatment for patients because it is non-surgical, has potential to eliminate snoring and obstruction, and can be used without significant side effects. Elimination of snoring causes an improvement in the spouse/partner’s sleep as well. However, recent studies show only about 40% mid-term compliance, or the will to maintain treatment. Nonetheless, some patients tolerate CPAP quite well over a long term. It is covered by most insurance companies.
Oral appliance therapy (OAT) is an alternative to CPAP and uses a nocturnal mouth guard to advance the lower jaw relative to the upper jaw and dilate the upper airway. It has a similar compliance rate to CPAP. Impossible to use in patients with dentures, teeth grinding, or TMJ, it nonetheless is well-tolerated in a minority of patients. With a prescription from a MD or DO for use in OSA, many insurance companies will cover the cost of the device when measured and constructed by a dentist.
Surgical options for OSA—Something you don’t have to wear.
A reasonable option for many people with OSA is surgery to improve the airway, which extends from the nostrils to the bronchioles. All forms of OSA are either thought or demonstrated to be due to an anatomic obstruction caused by abnormal anatomy or abnormal muscle tone in the setting of air flow and pharyngeal pressure changes. The upper airway is not a tube but a moving, elastic, variable, and highly complex space. When added to the changing complexity of the nasal airway, clearly considerable planning is necessary by the surgeon/patient team prior to surgery. The typical patient has more than one area of obstruction.
In terms of the oral and pharyngeal airway, it is critical to determine the precise locations for surgery. This is accomplished by utilizing Drug-Induced Sedation Endoscopy (DISE), 3-D reconstruction from CT or MRI scan data (virtual endoscopy), and/or careful orthognathic measurements on a lateral skull X-ray. Of these techniques, DISE is the most useful since it is a dynamic measurement and most closely approximates the conditions of sleep. In this procedure, conducted in the outpatient surgery center, a state of pseudo-sleep is induced with intravenous propofol. While asleep, the patient's upper airway is fiber-optically examined and a video file is created— indicating the specific areas of airway collapse—in order to plan the most effective and minimally invasive surgical procedure. Several days later, the specific surgery is planned with the patient and performed.
Is it Day or Night or Something Else?
Our bodies contain an internal clock (called the circadian rhythm) which controls our sleep/wake cycles dependent on various inputs including exposure to sunlight, levels of melatonin synthesized in the body, as well as other factors. The American Academy of Sleep Medicine estimates that more than 21 million US workers regularly work alternate shifts that fall at least partially outside the daytime/daylight shift range.
Rotating shift changes (day-night-day) adversely affect sleep quality in many workers. Rotating shift workers may experience significantly more difficulty with falling asleep and maintaining sleep, excessive sleepiness, higher work absenteeism and accidents, than those who work a fixed day or night shift.
Sleep deprivation is measured in terms of the time it takes you to fall asleep once your head hits the pillow. Times shorter than 7-10 minutes indicates that you are sleep-deprived. Chronic sleep deprivation may also occur in night shift workers who usually sleep 1 to 4 hours less than daytime workers. This leads to impaired social and cognitive function, as well as pathological sleepiness with safety and health hazards, including increased susceptibility to certain cardiovascular diseases and cancers.
Wake up!
Multiple studies have demonstrated that sleep disorders and especially uncontrolled obstructive sleep apnea leads to decreased life expectancy and the morbidity factors listed above. It has been associated with cognitive decline, accidents, and general decline in quality of life measures. At ENTA, we can help you avoid these tragic consequences.
Find an ENT & Allergy Associates Doctor Near You, or Explore More Blog Topics
